features and benefits
Improve inefficient claims feedback cycles
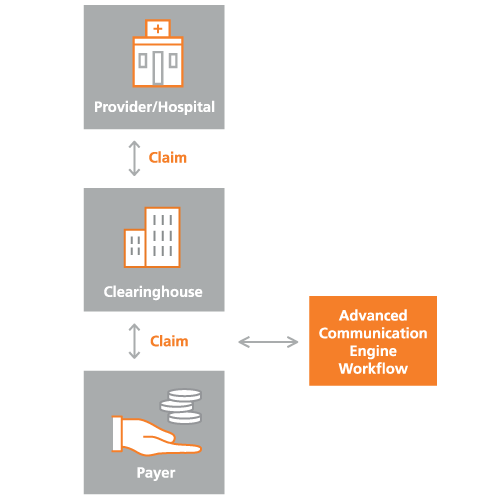
The Advanced Communication Engine (ACE) platform easily integrates with providers’ existing workflows, allowing health plans and third-party administrators to strategically insert clinical editing and analytic rules into their existing EDI clearinghouse workflow.
Correct claim errors before they reach you
Deliver timely feedback to providers on actionable errors or information gaps that often trigger claim denials. This level of prevention helps reduce manual rework, resubmission of denied claims, appeals and the back-and-forth communication between stakeholders.
Significantly reduce administrative costs
A minor coding error or duplicative claim leads to increases costs. Help move coding edits forward into the Electronic Data Interchange (EDI) stream without any additional administrative effort on your end.
Customize alerts and edits for your network
ACE includes eight categories of edits and analytics to be deployed into the EDI stream in a modular fashion:
- Clinical
- Eligibility duplicate
- Prior authorization
- Operational
- Attachment
- Administrative
- FW&A
- Quality analytics
Deliver balance value to all stakeholders
Empower providers to fix errors or omissions that cause claim denials The result is providers submitting accurately completed claims and health plans subsequently reducing claims-processing times that require costly investigation and recovery efforts.
Resources
Case study: Medicare claims processor reduces denials, strengthens provider relationships
